Some social and political commentators have focused on the DoD’s policies regarding transgender servicemembers. Much of the commentary has been heavily negative, frequently linking the military’s preoccupation with social issues1 like transgender policy with a decrease in its combat effectiveness. In this week’s article, I will focus exclusively on the DoD’s own policy documents. I’ll make a few observations which, I submit, flow directly and objectively from these documents. My intent is to avoid subjective comments or editorializing.
Please note: I am not arguing for or against transgenderism in this article. Here are the policy facts, from the DoD horse’s own mouth. And if you think that any of this reads as if the DoD’s transgender policies are arbitrary, inconsistent (even contradictory), unnecessarily convoluted, and illogical—well, then, I guess you’re a transphobe. And I assure you, none of this is a waste of the military’s resources or of taxpayer money.
Let’s start with Defense Health Agency (DHA) Procedural Instruction 6025.21, Guidance for Gender-Affirming Health Care of Transgender and Gender-Diverse Active and Reserve Component Service Members, dated 12 May 2023.
Pg. 8, Enclosure 2 (Responsibilities), Section 1.a:
DIRECTOR, DHA. The Director, DHA, will:
a. Provide or coordinate guidance and oversight, as appropriate, to standardize the provision of medically necessary health care for TGD [transgender and gender-diverse] ADSMs diagnosed with gender dysphoria (GD), including members for whom gender transition is determined to be medically necessary by a medical provider, in accordance with Reference (j).
This establishes that gender dysphoria (GD) is a medical condition—a disease state—with which one is diagnosed, and that there are cases when health care to treat this condition is medically necessary.
Pg. 10, 6.e:
6. DIRECTORS, DRM, SSO, AND DHAR. The DRM [Direct Reporting Markets], SSO [Small Market and Stand-Alone Military Medical Treatment Facility Organization], and DHAR [Defense Health Agency Regions] Directors will:
e. Ensure official recognition and allocation of sufficient protected time [emphasis added] for TGCT [Transgender Care Team] members to execute their assigned TG care duties either as primary or collateral duties.
And pg. 10, 7.c:
7. DIRECTORS, MTF [Medical Treatment Facility]. The MTF Directors will:
c. Provide sufficient protected time [emphasis added] to clinicians and designated personnel providing substantial TGD care support to execute their assigned duties.
Please note that no other DHA publication—and there are many of them—guarantees “protected time” for any purpose other than providing TG care. To confirm this, I searched the internal (access restricted) DHA site for any mention of the term “protected time”:
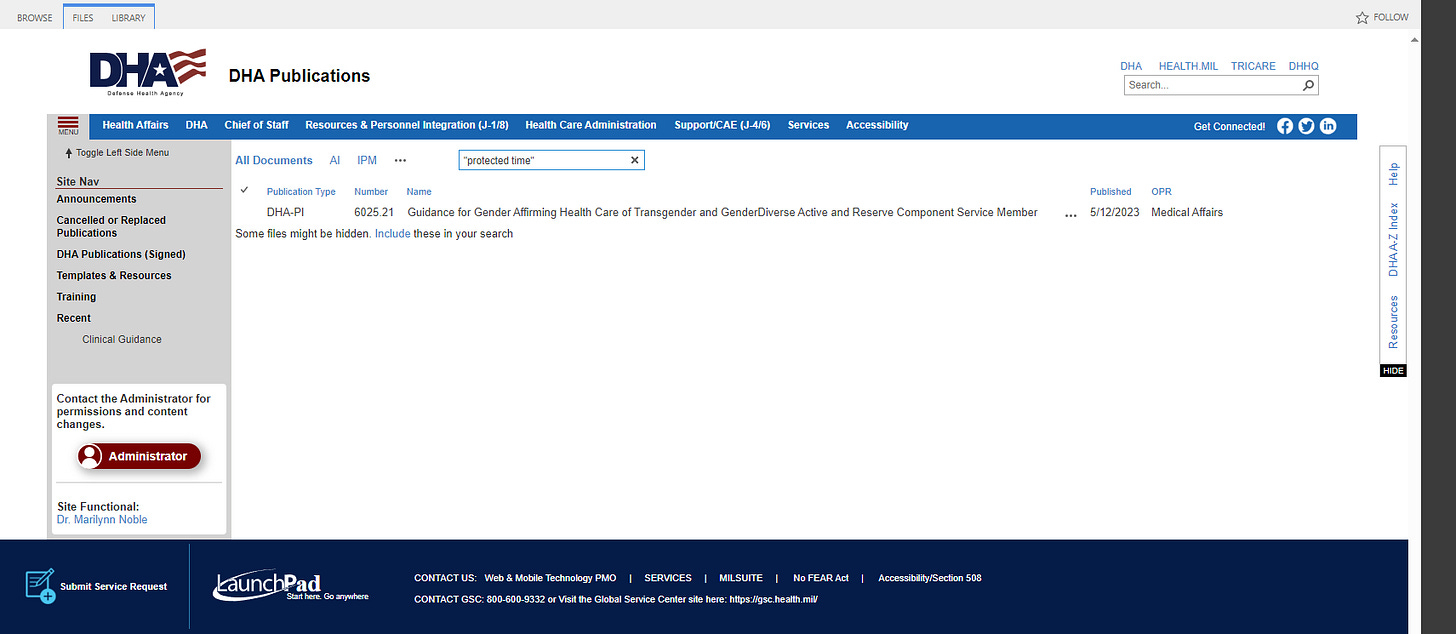
Anyone with CAC/PKI access can access this site to double-check my info.
Pg. 12, Enclosure 3 (Procedures), Section 1 and 1.a [emphasis added]:
1. GENERAL PROVISIONS. The MHS plays a critical role in establishing the diagnosis of GD/gender incongruence (GI) for in-service gender transition. This diagnosis has significant implications for the ADSM [Active Duty Service Member] and the ADSM’s immediate supervisor or commander and shall be made by providers who meet the recommended qualifications as specified in Reference (i).
a. Definitions. Transgender or TG is an umbrella term used to capture the spectrum of gender identity and gender-expression diversity. GI occurs when an individual’s sex assigned at birth and gender identity do not align, and the individual may identify as TGD. Some individuals experience GI at a clinically significant level, resulting in GD, specified in Reference (o) as a marked incongruence between one’s experienced or expressed gender and sex assigned at birth of at least six months’ duration and is associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Again confirming that GD/GI is a medical diagnosis that indicates a disease state that results in “clinically significant distress or impairment”, and adding that this diagnosis has “significant implications” both for the patient (ADSM) and the patient’s commander.
Pg. 13, Section 2.a.(3):
(3) All care for TGD ADSMs should be provided in the Direct Care System (DCS) to the extent appropriate. When gender-affirming care is not available in a given MTF, that MTF shall pursue the availability of the needed care in other MTFs before making referrals to the PSC [Private Sector Care, i.e., civilian healthcare organizations]. Telehealth should be utilized to coordinate and deliver care, where appropriate.
Military MTFs routinely refer specialty care to the private sector when it’s not available on base. No other type of healthcare in the military has this sort of injunction to provide the care in military MTFs, even if it’s remote/telehealth care, rather than referring to the private sector.
Pg. 17, Section 2.d.(3).(g): (emphases added)
(2) Roles of TGCT [Transgender Care Team]. The TGCT will:
(g) Ensure the disclosure of protected health information will be consistent with References (l) and (r). If an ADSM is diagnosed with GD/GI but does not require medications or procedures for this diagnosis (i.e., treatment plan consisting only of counseling with or without psychotropic medications), notification is not required. As in the treatment of any other mental health conditions, ADSMs’ commanders are notified only under specified circumstances, and with minimum necessary information, in accordance with Reference (m). Nothing in this DHA-PI affects the reporting requirements of Reference (m).
There are levels of GD/GI, and some of these levels do not require anything beyond counseling. GD/GI is a mental health condition.
Pg. 17, Section 2.f:
(1) GAS [gender-affirming surgery] may be a part of an ADSM’s gender transition MTP. GAS refers to all medically necessary surgical procedures associated with affirming the ADSM’s gender identity. These procedures are further categorized as procedures that do and do not affect fertility.
GD/GI is a mental health condition (see previous note) for which surgery may be medically necessary. No other mental health condition requires surgery as a medical necessity.
Pg. 20, Section 2.i:
i. Reversal of GAS. In accordance with Reference (j), if the reversal of GAS is determined to be medically necessary by a military medical provider treating the patient, or the TGCT, the ADSM will discuss and work with the PCM [Primary Care Manager] and the TGCT to establish a new MTP [Medical Treatment Plan] for the reversal of GAS procedure(s), and/or to alleviate unresolved or worsening GD, and the medical provider will implement the plan by referring the ADSM to a MTF with capability, or request for a SHCP [Supplemental Health Care Program] waiver for treatment not available in the MTF.
Surgery may not correct gender dysphoria, and may actually make it worse, in which case a whole new course of treatment needs to be prepared—up to and including reversal of surgery (which, depending on the nature of the initial surgery, may be purely cosmetic vs. functional).
Pg. 18, Section 2.g.(2).(a) and pg. 21, Section 3.e.(2) (Care for Non-Binary and Gender Diverse People)
2.g.(2).(a): (a) The ADSMs’ MTF providers may submit a referral for the pre-op surgical evaluation for fertility affecting GAS procedures after 9 months of GAHT [Gender-Affirming Hormone Treatment] (if indicated) and RLE [Real-Life Experience, meaning “living as a person of the opposite gender”], as documented in the ADSM’s Electronic Health Record.
3.e.(2):
3. CARE FOR NON-BINARY AND GENDER DIVERSE PEOPLE
e. The recommendations in Reference (s) for this population are:
(2) Consider gender-affirming medical interventions (hormone therapy or surgery) for non-binary people in the absence of “social gender transition” (i.e., RLE).
A transgender person must go through 9 months of hormone treatments and living as a person of the opposite gender before being considered for surgery. But a non-binary person may be considered for surgery without any of these prior requirements.
Pg. 21, Section 3.c:
c. As stated in Reference (s), the medical treatment needs of non-binary people are particularly diverse, and the more common transition trajectories historically associated with transgender men and women may not align with the way many non-binary and gender diverse people understand themselves and their personal transition process. Therefore, common treatments, or combination of treatments, often seen in the health care of TGD men and women, may not be indicated for the non-binary and gender diverse population, and thus those treatments’ associated eligibility criteria may not be applicable or appropriate for the non-binary and gender diverse population.
Gender transition is a trajectory. It may follow a simple linear course, or may describe a parabola through curved time-space—which we prefer to call the vagina-penis continuum. Most conventional depictions of the vagina-penis continuum use three vagina-like dimensions and one penis-like dimension. However, there is a concept known as “super-tampon-string theory” which posits multiple other dimensions that are curved in upon themselves through surgical “rearrangement”.
Pp. 22-23, Sections 4.a.(2)-(4) [emphasis added]
4. MEASURES OF COMPLIANCE AND REPORTS. The TGHWG [Transgender Health Working Group], in collaboration with the TGHC, will work with MILDEPS [Military Departments] and SMEs [Subject Matter Experts], as needed, to obtain the following information at the minimum once a calendar year.
a. Cohort Characteristic
(2) The number of psychotherapy encounters and associated costs of ADSMs with
GD/GI per calendar year;
(3) The number of GAHT prescriptions and the associated costs; and
(4) The number of GAS procedures performed for ADSMs, and the associated costs.
This diagnostic group explicitly requires regular reporting of its costs. I’m not aware of any other diagnosis that requires this sort of accounting.
Pg. 23, Section 5.a:
a. Introductory TG Healthcare Training
(1) This training will be completed once by all MTF personnel including military, civilians, and contractors.
(2) Training is required upon publication of new training modules, revision of this DHA-PI or related policy guidance, and new staff onboarding without prior TGD healthcare training.
The rest of the Section outlines the training requirements. Every single person who works in any treatment facility in the Military Health System, regardless of position, must receive this training.
Pg. 26, Enclosure 4 (Surgical Procedures in Transgender Health Care, Section 1.a [emphasis added]:
a. For surgical procedures directly affecting fertility, the endocrinologist, or physician responsible for endocrine treatment, certifies the ADSM has continuously and responsibly used gender-affirming hormones for 12 months (unless hormone therapy was not desired or part of the MTP, or was medically contraindicated), and has engaged in 12 months of RLE as determined by the TGHC, or designated TGCT, to meet recommended clinical criteria per Reference (i). Referral for a GAS surgical evaluation may be submitted and completed at any point during or after the 9th month of continuous adherence to the general criteria listed in Table 1, as specified in Enclosure 3 of this DHA-PI;
Before surgery, the patient must undergo hormone therapy and live as the opposite gender for at least 12 months. Unless the patient doesn’t want hormones, in which case this requirement doesn’t apply. Or unless the patient is non-binary or gender-diverse (see above), in which case this requirement also doesn’t apply.
Pg. 26, Section 2:
2. COMMANDER’S REVIEW OF GAS PROCEDURES. The ADSM’s line or operational commander is responsible for approving the timing of any medically necessary surgical procedure(s) to minimize any possible impact on unit readiness.
It’s the commander’s job to figure out how to deconflict gender-affirming surgery with operational requirements. This is common with elective surgical procedures, where the timing of the surgery is flexible. This is not normal for medically necessary surgical procedures; if something’s medically necessary, it’s scheduled at a medically appropriate time, and everything else adjusts to accommodate.
Pp. 27-29, Table 1 (Fertility Affecting Gender Affirming Surgical Procedures), and pp. 29-30, Table 2 (Non-Fertility Affecting Gender Affirming Surgical Procedures). I won’t reproduce the tables here, but have a read for yourself. Some of my favorites [emphases added]:
Phalloplasty (construction of “new” penis from skin or muscle grafts) 58999: Unlisted procedure, female genital system (nonobstetrical)
Placement of testicular prostheses 54660: Insertion of testicular prosthesis (separate procedure)
Scrotoplasty (re-arrangement of labia to create scrotum) 55175: Scrotoplasty; simple, 55180: Scrotoplasty; complicated
Urethroplasty (creation of longer urethra from skin to enable standing voiding) 53430: Urethroplasty, reconstruction of female urethra
Penectomy (removal of penis) 54125: Amputation of penis; complete
Vaginoplasty (construction of “new” vagina from skin or intestinal tube) 57291: Construction of artificial vagina; w/o graft, 57292: Construction of artificial vagina; with graft
Clitoroplasty (rearrangement of penile tissues to create “new” clitoris) 55899: Unlisted procedure, male genital system
Labiaplasty (rearrangement of scrotum to create “new” labia) 55180: Scrotoplasty; complicated, 55899: Unlisted procedure, male genital system
Gender-affirming voice training 92700: Unlisted otorhinolaryngological service or procedure
Some of these have no code associated with the procedure; I guess the medical system just hasn’t caught up. There’s a surgical procedure that makes a female urethra longer so that she (soon “he”) can urinate while standing. Quite a bit of “rearranging” going on. You need to have guts to have a new vagina installed (but you’ll have a little less guts after).
Pg. 30: “FFS [Facial Feminization Surgery] is performed only in DCS [Direct Care System, i.e. military hospitals, not civilian facilities].”
There exists a “Facial Feminization Surgery”, but no “Facial Masculinization Surgery”. FFS can only be done in military MTFs, unlike every other listed procedure.
Pg. 32, Enclosure 5 (COSMETIC AND OTHER NON-COVERED PROCEDURES), Section 3:
3. EXCEPTIONS
a. A SHCP waiver for breast augmentation may be authorized on a case-by-case basis when the ADSM has undergone 24 months of feminizing hormone therapy with insufficient breast development, as advised in Reference (i) (unless medically contraindicated).
b. Facial bone reduction surgical procedure(s) and other procedures for FFS may be authorized in the DCS only when the TGCT considers this procedure to be medically necessary for the patient, and is thus not eligible for a SHCP waiver.
c. Reduction thyroid chondroplasty (i.e., Adam’s Apple surgery) for trans feminine patients may be authorized in DCS when the TGCT considers this procedure to be medically necessary for the patient.
Cosmetic procedures are not covered, except when they are.
Pg. 35, Enclosure 7 (SHCP GAS PROCEDURE WAIVER GUIDANCE), Section 2.a:
2. DOCUMENTATION.
a. The referring provider must use the DHA Form 233, “Gender-Affirming Surgery Waiver Form,” to develop the GAS waiver request package. GAS SHCP waiver requests must utilize DHA Form 233. Requests submitted without DHA Form 233 will be returned.
DHA has created a form, DHA Form 233, for the sole purpose of requesting approval to get gender-affirming surgery in a civilian hospital. I wonder how many full-time employees at DHA do nothing but create and retire forms. No other diagnostic group has a dedicated form and review process for requesting approval to have it done in a civilian hospital; a simple referral is enough for anything except GAS.
Pg. 36, Section 2.b.(11) [emphasis added]:
b. The GAS SHCP waiver request requires specific information and documentation, depending on the type of GAS is being requested. Reference Form 233 for detailed information. Some of the required information, for example, includes (but is not limited to) the following:
(11) Relevant contingency restrictions, such as Coronavirus Disease 2019, pre-op testing limitations, limitation on availability of elective procedures, and concerns with post-operation inpatient stays in locations with high transmission rates, etc.
Those who want their gonads removed and their genitalia surgically “rearranged” must report if they intend to done something risky, like get the procedure done in an area with high COVID transmission rates.
Pg. 38, Appendix (MEDICAL TREATMENT PLAN TEMPLATE):
The following interventions are medically necessary:
☐ Social Transition: The following Exceptions to Policy (ETP) support social transition and are recommended beginning upon submission of an ETP request by the SM:
☐ Dress and appearance
☐ Facilities/Berthing/Billeting
☐ Fitness Standards
☐ Military Personnel Drug Abuse Testing Program
☐ Body Composition Program
Working backwards, it may be medically necessary to allow servicemembers to:
Violate Body Composition Program standards (body fat)
Be exempt from drug testing
Meet lower fitness standards (female fitness requirements are universally lower than male ones)
Cohabitate with their new gender
Conform to the grooming standards of the other gender
So biological men in the US military are not allowed to wear a neatly trimmed beard, but it may be medically necessary for them to look like this:
Now let’s move on to Department of Defense Instruction (DoDI) 6130.03-Volume 1, MEDICAL STANDARDS FOR MILITARY SERVICE- APPOINTMENT, ENLISTMENT, OR INDUCTION and DoDI 6130.03-Volume 2, MEDICAL STANDARDS FOR MILITARY SERVICE- RETENTION.
Vol. 1 contains the standards one has to meet to join the military, whereas Vol. 2 contains the standards to stay in the military. Generally, retention standards are lower because once you’re in, the military is invested and wants to keep you if possible—even if you’re not in tip-top shape any longer.
We’ll start with the obvious.
Vol. 1 (initial entry standards), Section 6 (Disqualifying Conditions), Subsection 6.28 (Learning, Psychiatric, and Behavioral Disorders), pg. 52:
t. History of gender dysphoria if:
(1) Symptomatic within the previous 18 months; or
(2) Associated with comorbid mental health disorders.
NOTE: there is no entry for “gender incongruity”, although GI appears as a mental health condition in DHA-PI 6025.21, the document reviewed in the first part of this article. A diagnosis of “gender dysphoria” is disqualifying for entry into the Armed Forces if it’s been symptomatic within the last 18 months or if it’s associated with any other mental health condition, such as depression or anxiety. But then again, what are the odds that a gender dysphoric patient—clearly, a well adjusted individual—has any of those comorbidities?
For reference, either of these mental health comorbidities is disqualifying if symptomatic within 36 months. If you’ve felt like you were trapped in a body of the wrong biological sex 18 months and 1 day ago, you’re fine (although you might need to have your genitalia surgically “rearranged”); but if you were sad or worried on that same day, you’re disqualified.
Pg. 51:
f. Depressive disorder if:
(1) Outpatient care including counseling required for longer than 12 cumulative months;
(2) Symptoms or treatment within the previous 36 months;
(3) The applicant required any inpatient treatment in a hospital or residential facility;
(4) Any recurrence; or
(5) Any suicidality (in accordance with Paragraph 6.28.m.).
Pg. 52:
q. History of anxiety disorders if:
(1) Outpatient care including counseling was required for longer than 12 cumulative
months.
(2) Symptomatic or treatment within the previous 36 months.
(3) The applicant required any inpatient treatment in a hospital or residential facility.
(4) Any recurrence.
(5) Any suicidality (in accordance with Paragraph 6.28.m.).
Vol. 2 (retention standards), Section 5 (Disqualifying Conditions), Subsection 5.28 (Behavioral Health), makes no specific mention of GD/GI. There is a brief “catch-all” paragraph on pg. 36:
d. Other behavioral health conditions, defined using the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders—including, but not limited to, anxiety disorders, depressive disorders, or eating or feeding disorders—will be considered on a case-by-case basis if, despite appropriate treatment, they:
(1) Require persistent duty modifications to reduce psychological stressors or enhance safety; or
(2) Impair function so as to preclude satisfactory performance of required military duties of the member’s office, grade, rank, or rating.
One must assume that berthing with a new gender2, being subject to different fitness standards, and being exempt from drug testing (all potential medically necessary interventions per DHA-PI 6025.21) do not constitute “persistent duty modifications”.
Vol. 1 (initial entry standards), Section 6 (Disqualifying Conditions), Subsection 6.13 (Female Genital System), pg. 29:
g. History of urogenital reconstruction or surgery (including, but not limited to, gender-affirming surgery), if:
(1) A period of 18 months has not elapsed since the date of the most recent surgery;
(2) Associated with genitourinary dysfunction or recurrent urinary tract infection;
(3) Associated with functional limitations of activities of daily living or a physically active lifestyle; or
(4) Additional surgery is anticipated.
Vol. 1 (initial entry standards), Section 6 (Disqualifying Conditions), Subsection 6.14 (Male Genital System), pg. 30:
n. History of urogenital reconstruction or surgery (including, but not limited to, gender-affirming surgery), if:
(1) A period of 18 months has not elapsed since the date of the most recent surgery;
(2) Associated with genitourinary dysfunction or recurrent urinary tract infection;
(3) Associated with functional limitations of activities of daily living or a physically active lifestyle; or
(4) Additional surgery is anticipated.
All of the above supports the previous eligibility criteria related to GD: acceptable, as long as it’s not within the last 18 months.
Vol. 2 (retention standards), Section 5 (Disqualifying Conditions), Subsection 5.14 (Male Genital System), pg. 20:
a. Absence of both testicles with medically required injectable hormone therapy.
This appears to disqualify any biological male who has undergone the following procedure and also requires hormone therapy, to include gender-affirming hormone therapy:
Orchiectomy (removal of testicles) 54520: Orchiectomy, simple (inc.subcapsular),w/wo testicular prosthesis, scrotal/inguinal approach or 54690: Laparoscopy, surgical; orchiectomy
Astute readers will recognize this entry from DHA-PI 6025.21 (Guidance for Gender-Affirming Health Care of Transgender and Gender-Diverse Active and Reserve Component Service Members), Enclosure 4 (Surgical Procedures in Transgender Health Care), Section 3 (Medically Necessary Procedures), Table 1 (Fertility Affecting Gender Affirming Surgical Procedures).
I’m not saying that the Defense Health Agency is wasting time and money by writing detailed policy documents that accommodate a negligible percentage of the force. Nor am I saying that they should instead be spending all that time and money on providing healthcare to, and ensuring the medical readiness of, the remaining vast majority of its force. I can’t possibly be saying that the tail is wagging the dog, and that the juice isn’t worth the squeeze. And I’m definitely not saying that it might not be strictly necessary to train every single member of the Military Health System on how to provide healthcare that’s specifically tailored to transgender (or non-binary, or gender-diverse) individuals, especially when the information to be trained on is as convoluted and self-contradictory as the above.
I’m just saying: this is what your tax dollars are paying for.
I look forward to publishing this article in Mandarin in about ten years. Nǐ hǎo!
To be fair, it’s not the military’s choice to be so preoccupied; they have to do it in order to satisfy the demands of Congresscreatures who link their pet social projects to military funding bills.
Note: in a contingency / operational environment, where every bed and bathroom space is accounted for, a change in the male-female ratio is not insignificant and requires additional logistical planning.





Remember when lobotomies were required for mental health issues that were unresponsive to other treatment? Pepperidge Farm remembers.
After hearing about the problems in female prisons due to men identifying as women, I’m glad I am no longer part of an institution that could potentially force me to sleep and shower in a place where a man might also prefer to be.
Look, go be your fabulous self if you want- on your own dime. I’m all for the liberty to choose how one lives their life. However, these sort of policies don’t belong in an institution where there needs to be a high level of trust. Members of the military expect their coworkers to be fit, healthy, of a sound mind, and focused on the mission. They expect to be able to trust the people they have to share a dorm, barracks, ship, or tent, foxhole etc with. Given that we reject so many people who want to serve with less issue than GD, it seems insane that our government would put so much time, effort, and money into a program that serves a small population, doesn’t always help that population, and causes logistical problems when it comes to the personnel/ mission that person is assigned with/to.
wow...